- Care solutions
- Home Care
- Residential Care
- Retirement Villages
- Dementia Care
- Disability Services – NDIS
- Respite Care
- What is Aged Care?
- Health & Wellbeing
- Our Locations
- Careers
- About Whiddon

The Collaborative Health Care (CHC) Initiative is a multi-sector partnership focused on improving health and aged care for older Australians in rural and regional communities through better integration of care, resource sharing, and collaborative governance. This provider-led initiative brings together a broad coalition of stakeholders including aged care providers, federal and state health departments, peak bodies such as Ageing Australia and the National Rural Health Alliance, and academic experts.
Demonstrating a commitment to rapid and effective action, the collaborative has held two national workshops over three months, resulting in the development of six pilot projects now moving into implementation.
Collaboration between State and Federal Health Services, allowing Local Health Districts (LHDs) and aged care homes to share resources, including joint staffing across hospitals and care homes, and shared services between co-located or nearby facilities. This aims to reduce competition, increase operational efficiencies and improve service delivery for better community outcomes.
An integrated approach that delivers coordinated care pathways that enable better discharge planning, community-based support, and continuity of care for our elderly living in rural and remote communities. Including programs that allow hospital patients to participate in wellbeing activities at aged care homes and streamlined access to transitional aged care beds to reduce hospital bed block.
Bringing together the current fragmented and confusing system with cross-sector working groups and consultative structures to manage pilots and oversee the strategic approach. Employing flexible, non-bureaucratic oversight that allows for local responsiveness and joint decision-making, with evaluation driven by the University of Sydney, using evidence-based models.
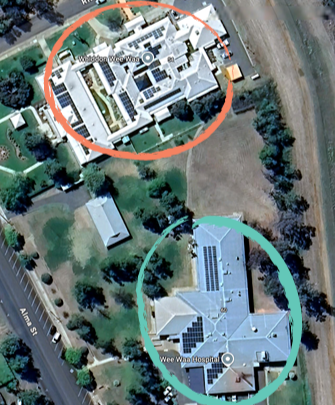
In regional towns such as Temora, Narrabri, Kyogle, and Wee Waa, Whiddon’s homes sit side by side with health services, a scenario mirrored by many other aged care providers in rural and remote areas.
The CHC Initiative addresses the need for coordinated action by facilitating partnerships between nearby LHDs and aged care homes to share critical resources, such as Registered Nurses (RNs), care staff, and allied health professionals, as well as facilitating a reimagined transitional aged care model.
The initiative also suggests shared services for lifestyle and wellbeing programs, transport, catering, laundry, and maintenance operations, as well as emergency and disaster preparedness and response frameworks.
CHC Partners have identified and prioritised key challenges facing regional, rural, and remote communities. Across two workshops, they have co-designed solutions that will be piloted and evaluated in the coming months.
With a focus on real-world service integration and shared resources, these pilots aim to demonstrate how more agile, responsive systems can be built around community needs and local solutions. The projects will be designed to ensure learnings can be scaled across other regions, with the goal of creating sustainable impact nationally.

Leveraging an integrated approach between State and Commonwealth funded services, to provide elderly hospital inpatients with opportunities to engage in meaningful activities with residents at the local Care Home. With the aims to keep patient minds and bodies active, thereby reducing the deterioration often associated with hospitalisation.

A shared services employee model between aged care providers and the State Health system to optimise workforce resources, improve continuity of care, and reduce duplication. This model is increasingly relevant in rural, remote and resource-limited areas where demand for skilled healthcare workers is high.

To provide a seamless and supportive transport service for older hospital inpatients, and residents of Residential Care Homes to attend their medical appointments. The project will involve home care staff, providing transport to hospital patients and residents of aged care who are otherwise unable to access or afford transport.

Working collaboratively to deliver high level outcomes for aged care residents and hospital patients, through shared non-clinical services. These services include food, laundry and maintenance, while realising operational efficiencies for all stakeholders, and combating staff shortages.

A reimagined transitional aged care model that is collaborative, flexible, and agile in funding. It enables hospitals to discharge patients directly into residential aged care homes at a fixed daily rate, without the administrative burden of grant applications or rigid eligibility criteria. Designed to reduce hospital bed blockages, improve continuity of care, and enhance outcomes.

With an increasing number of adverse and severe weather events impacting rural and regional communities, this pilot aims to enhance emergency preparedness and response through a collaborative framework that ensures the continuity of care, safety of residents and patients, and effective use of local resources.
Currently, Australia’s healthcare system is fragmented, with state-based and federally-funded services often working in isolation and even in competition. This disjointed approach leads to inefficiencies, resource shortages, and poorer health outcomes for individuals living in rural and remote areas.
Further intensifying the issue is the growing population in regional Australia, with more than 600,000 people relocating to rural and regional communities following the COVID-19 pandemic.
The initial vision was outlined by Whiddon CEO Chris Mamarelis, who authored the Introductory Report, Oct 2024 calling for reform and locally driven, place-based solutions for regional care after witnessing these challenges first-hand.

"Our model shows how aged care providers and health services can pool resources to deliver better outcomes for the community.
This isn’t just about providing operational efficiencies —it’s about ensuring continuity of care and enhancing the quality of life for people in regional Australia."
Whiddon publishes Collaborative Health Care Model Introductory Report, Oct 2024, proposing shared care solutions for regional Australia.
Stakeholder outreach and initial planning with Nous Group and University of Sydney.
Workshop One: Hosted at University of Sydney; stakeholders from DOHAC, NSW Health, peak bodies and providers agree on shared vision and 4 priority pilot areas.
Interim Report, June 2025 drafted; key pilot sites scoped, and governance frameworks developed.
Workshop Two: Finalisation of pilot programs, locations, and working groups.
12-week pilot implementations begin at identified sites (Lithgow, Wee Waa, Casino, etc.).
Data collection, early evaluation, and refinement of models.
Outcomes presented to state and federal ministers.
Case studies published; CHC positioned for regional/national scale-up.